Osteoarthritis is the most common form of arthritis. Content on this page has been created to help people with knee osteoarthritis understand more about the condition.
We recommend that you watch the short video below that will take you through the basics. You may also find more specific answers to your learning needs in the FAQ section below.
If you’d like to test you knowledge about knee osteoarthritis before reading our content then click the icon on the left to go to our quiz!
Otherwise, watch the video below to start!
Download our ‘Facts & Fiction’ sheet here
Frequently Asked Questions (FAQs)
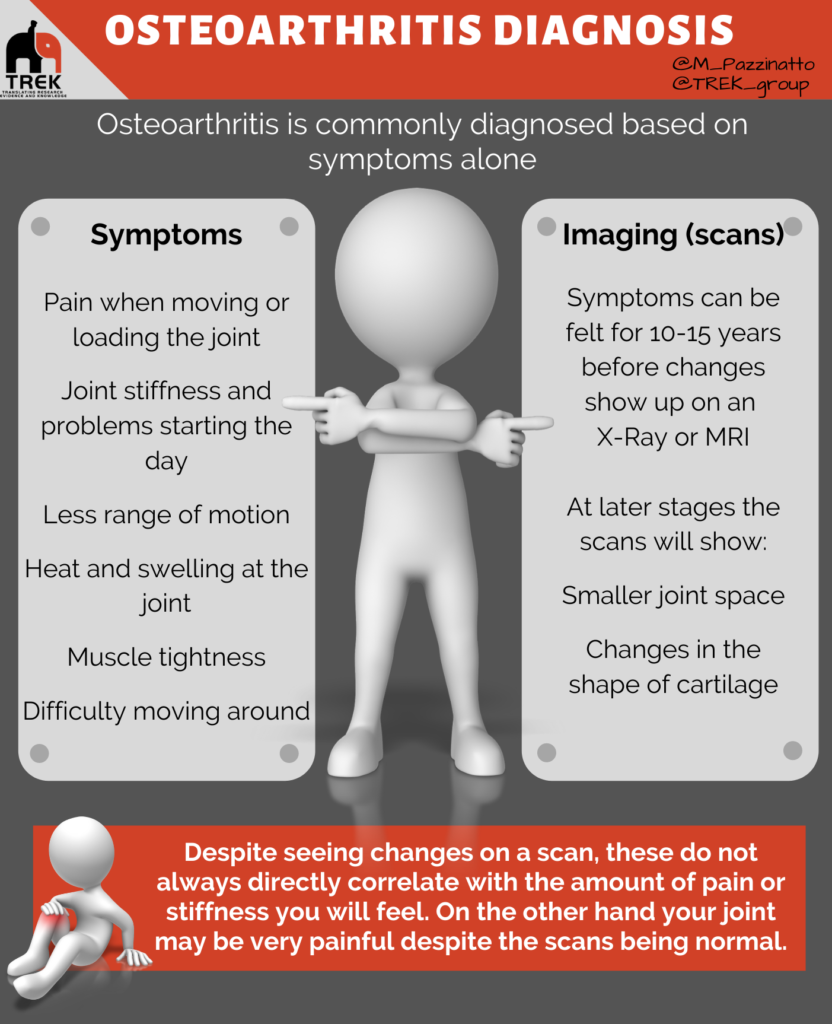
 We used to think that osteoarthritis was all about the bones and its coverings (articular cartilage). But we now know that the condition is far more complex than we once thought.
We used to think that osteoarthritis was all about the bones and its coverings (articular cartilage). But we now know that the condition is far more complex than we once thought.
For example, research has identified that osteoarthritis also affects structures like ligaments, nerves and muscles, plus there are overall changes to the inflammation process at the joint.
Also – we used to think that pain was directly associated to changes at the knee joint. For example, the ‘thinner’ your cartilage was, the worse your osteoarthritis or pain was. But this isn’t the case. There are many different factors that affect someone’s symptoms.
As a result, terms such as ‘bone on bone‘ and ‘wear and tear‘ are inaccurate and should not be used to describe the condition.
The OsteoArthritis Reseach Society International (OARSI) Provide the following definition of osteoarthritis:
“Osteoarthritis is a disorder that can affect any moveable joint of the body, for example knees, hips, and hands. It can show itself as a breakdown of tissues and abnormal changes to cell structures of joints, which can be initiated by injury. As the joint tries to repair, it can lead to other problems.
Osteoarthritis first shows itself as a change to the biological processes within a joint, followed by abnormal changes to the joint, such as the breakdown of cartilage, bone reshaping, bony lumps, joint inflammation, and loss of joint function. This can result in pain, stiffness and loss of movement. There are certain factors which make some people more vulnerable to developing osteoarthritis, such as genetic factors, other joint disorders (such as rheumatoid arthritis), injury to the joint from accidents or surgery, being overweight or doing heavy physical activity in some sports or a person’s job”.
 Osteoarthritis is the most common form of arthritis. There are other forms of arthritis (for example rheumatoid arthritis), but these are less common.
Osteoarthritis is the most common form of arthritis. There are other forms of arthritis (for example rheumatoid arthritis), but these are less common.
Osteoarthritis most commonly affects the knee joints, but also frequently affects the hips finger joints and big toes.
Did you know?
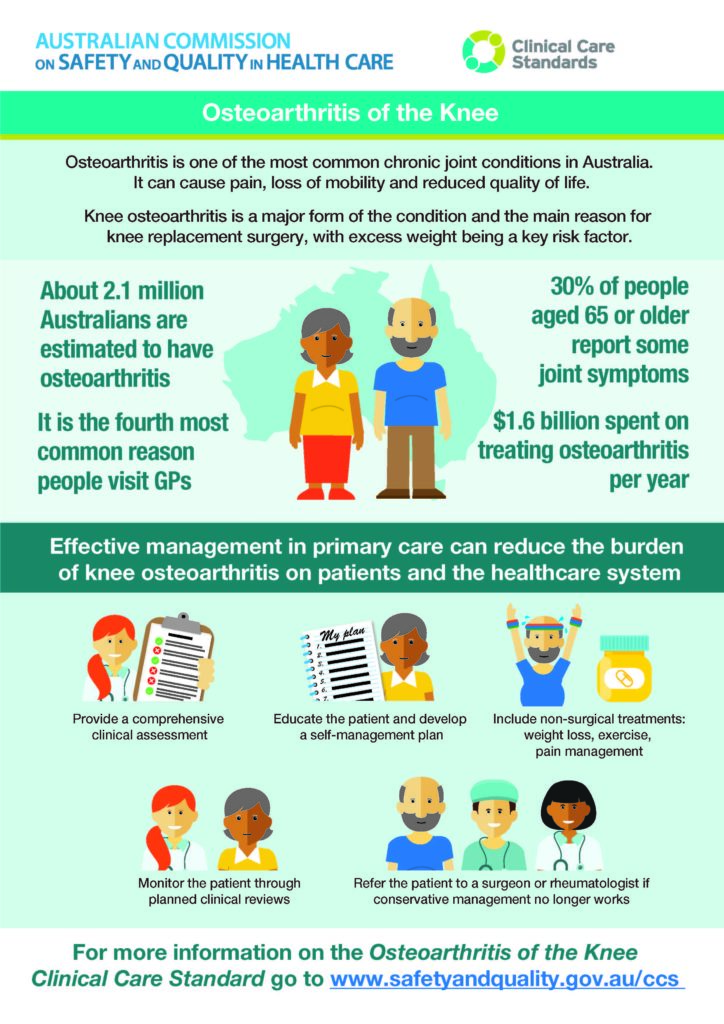
1 in 5 people over the age of 45 have osteoarthritis. The percentage of people who have osteoarthritis increases as age increases.
Younger and middle-aged people can also get osteoarthritis. Approximately 5% of people between 35 and 54 years of age have osteoarthritis. Many of these people have injured their joint earlier in life.
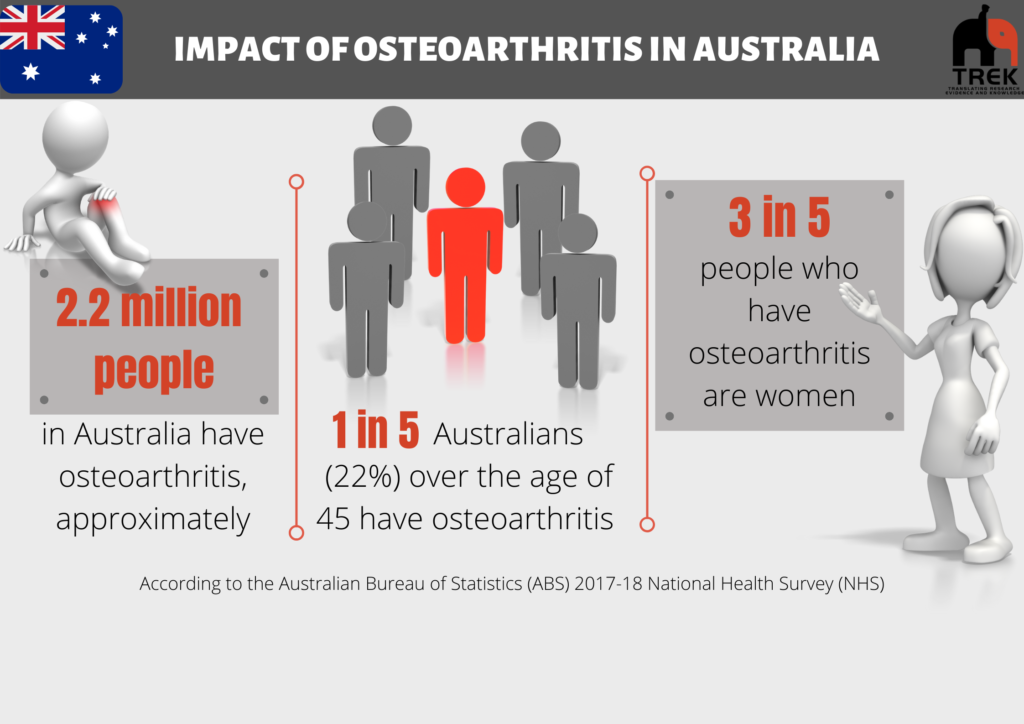
 Knee osteoarthritis can be diagnosed by your Doctor or another health professionals (i.e. a physiotherapists) clinically without the need for further scans (e.g. x-Ray).
Knee osteoarthritis can be diagnosed by your Doctor or another health professionals (i.e. a physiotherapists) clinically without the need for further scans (e.g. x-Ray).
x-Ray’s used to be a common way to diagnose osteoarthritis, but now that we understand more about the condition, we realise that they are not needed (and can sometimes even be misleading!).
A clinical diagnosis is now what is recommended in all guidelines for Doctors and health professionals.
This means that a Doctor or other health professional can diagnose your knee osteoarthritis just by you reporting what symptoms you are experiencing.
The criteria that was developed by the National Institute for Health and Care Excellence (NICE) in the U.K. is most commonly used. It states that someone has knee osteoarthritis if they:
- Are aged 45 years or older
- Have activity related joint pain
- Have either no morning stiffness or stiffness that lasts no longer than 30 minutes
There are other criteria available. For example, there are specific criteria for people with ‘early-onset osteoarthritis’. Speak with your doctor or health professional to find out more.
Did you know that the amount of ‘degeneration’ or ‘joint space narrowing’ on an x-Ray
- Does not accurately predict how severe someone’s pain or symptoms are
- Does not accurately predict whether someone can improve their symptoms or not
These are some reasons why x-Rays are less commonly used to diagnose knee osteoarthritis and why the terms ‘bone on bone‘ or ‘wear and tear‘ are inaccurate and should not be used to describe the condition..
Watch the below video to find out more
There is not one simple reason why you may have osteoarthritis – it is more likely a combination of non-modifiable and modifiable factors.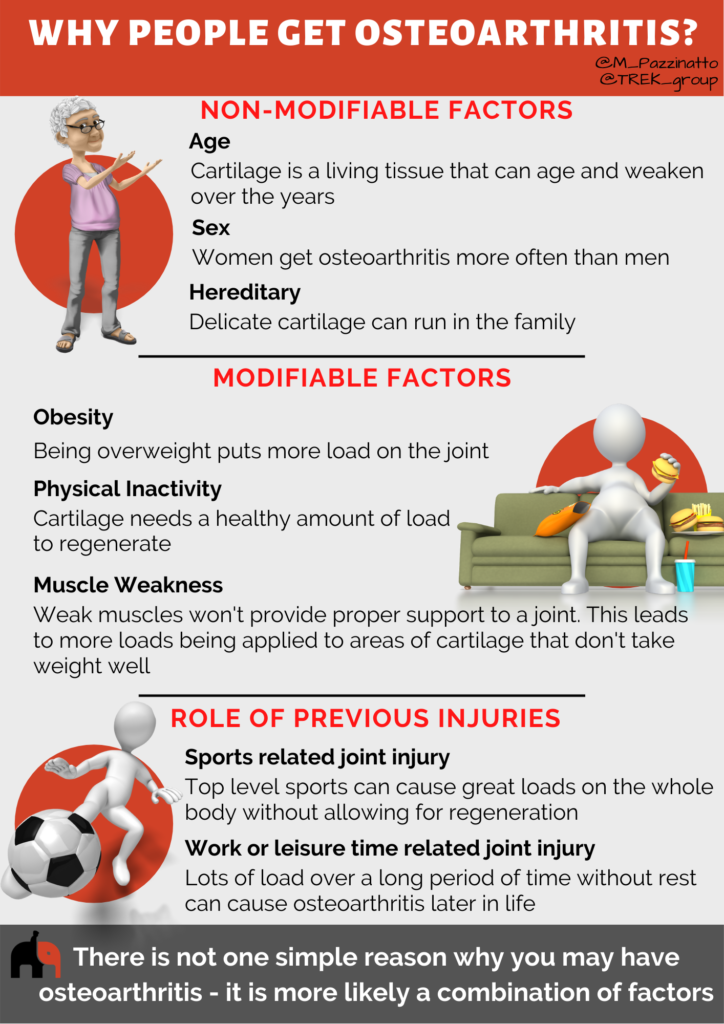
Non-modifiable factors (i.e. things that you can’t do anything about)
- Age – Cartilage is a living tissue that can age and weaken over the years. Osteoarthritis can happen at the early age of 30. However, people are more likely to have osteoarthritis after the age of 50.
- Sex – Women get osteoarthritis more often than men. Women get osteoarthritis more often in the knees and hands. Men get osteoarthritis more often in the hips.
- Genetics – Osteoarthritis can run in the family. So, you are more likely to get osteoarthritis if someone in your family had it too.
Modifiable factors (i.e. things that you can/may be able to do something about)
- Obesity – Not only can being obese put more load on the knee joint, but research also indicates that obesity is associated with changes to inflammation in the body that is thought to make someone more likely to develop knee osteoarthritis.
- Physical Inactivity – Not getting enough activity is another factor that makes someone more likely to develop knee osteoarthritis. Like obesity, the role of physical inactivity in knee osteoarthritis is complex. The knee joints need activity and ‘loading’ to keep the joint healthy. Little or no load of your knee joints therefore is bad for your knee joints and surrounding muscles.
- Muscle weakness – Weak muscles won’t provide proper support to your knee joint and make it more likely that you will develop knee osteoarthritis.
Did you know that… the modifiable factors listed above are also linked to making your knee osteoarthritis worse if you already have it. This is why first-line treatments for people with knee osteoarthritis involves education, exercise and weight management. Click here to find out more about treatments.
What about other factors?
- Sports related joint injury – Half of all people with a severe knee injury (meniscus or cruciate ligament injury), often from sports, get osteoarthritis 10-15 years later. Most people hurt their knee as a teenager, which means that they can get osteoarthritis in their 30s. Top level sports can cause great loads on the whole body without allowing for regeneration. This can lead to degeneration of cartilage.
- Work or leisure time related joint injury – Lots of load over a long period of time without rest can cause osteoarthritis later in life. People who work as labourers (farmers, firefighters, etc.) are more at risk of hip and knee osteoarthritis.
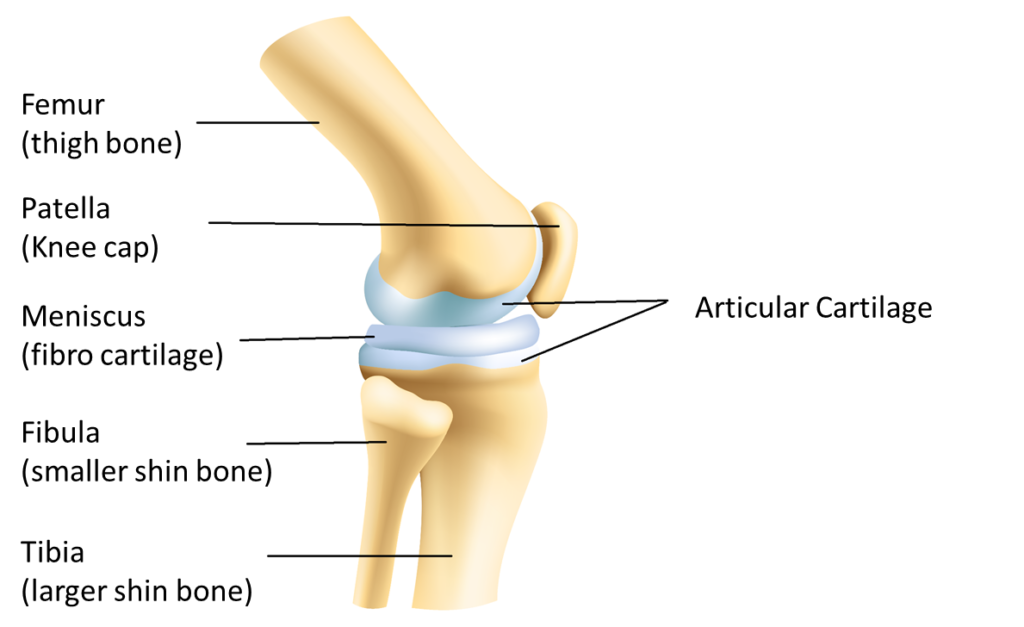 The knee joint is made up of a number of structures. The main bone and joint surfaces are shown in the diagram to the right.
The knee joint is made up of a number of structures. The main bone and joint surfaces are shown in the diagram to the right.
Most people think of the ‘knee joint’ being between the femur and the tibia (also known as the tibiofemoral joint).
There is another joint between the patella and the femur. This is known as the patellofemoral joint.
The ends of the femur and tibia, and the back surface of the patella are covered in ‘articular cartilage’. Its role is to help smooth movement between the bones.
There is also a layer of ‘fibrocartilage’ in between the tibia and the femur. You may hear this fibrocartilage being called the knee ‘meniscus’. This structure helps with shock absorption and also how well the bones move and fit together.
Its important to remember that joints also have other structures like a joint capsule and ligaments, plus the joint is surrounded by other structures such as nerves, muscles and tendons. All of which can be affected by osteoarthritis.
Resources and additional information
- Moore KL, Dalley, A.F. & Agur, A.M.R. Clinically oriented anatomy. 6the Edition ed. Philadelphia: Lippincott Williams & Williams; 2010.
- Mobasheri A, Batt M. An update on the pathophysiology of osteoarthritis. Annals of physical and rehabilitation medicine. 2016;59(5-6):333-339.
- National Clinical Guideline C. National Institute for Health and Clinical Excellence: Guidance. In: Osteoarthritis: Care and Management in Adults. London: National Institute for Health and Care Excellence (UK)
- French SD, Bennell KL, Nicolson PJ, Hodges PW, Dobson FL, Hinman RS. What do people with knee or hip osteoarthritis need to know? An international consensus list of essential statements for osteoarthritis. Arthritis care & research. 2015;67(6):809-816.
- Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323-1330
- Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105(1):185-199.
Next – Understanding symptoms